Seeking to Improve Quality of Life for Children with Achondroplasia
For children with achondroplasia, the most common type of dwarfism, scientists are exploring new ways to restore bone growth and potentially address some of the major health complications with the condition, such as spinal problems, swelling in the brain, frequent ear infections and sleep apnea.
Achondroplasia is a rare genetic bone disorder affecting 1 in 15,000 to 40,000 people in the U.S. The average height for men with the condition is about 4 feet, 4 inches and for women it’s 4 feet, 1 inch. However, it is the short arms and legs in proportion to the torso that can cause significant issues, as well as complications related to the head, neck and spine. There is currently no therapeutic option for children born with the condition.
But now, with recent research advances, scientists at Pfizer are working to develop a biologic medicine that targets mutated fibroblast growth factor Receptor 3 (FGFR3), a signaling pathway that causes decreased bone growth in achondroplasia. Pfizer acquired this candidate compound through its acquisition of Therachon, a biotech company based in Basel, Switzerland, in May 2019. Therachon is planning to enter into phase II clinical trials in late 2020, testing with its first group of pediatric patients. “We want to treat as early as possible in childhood,” says Christian Czech, Senior Director, Head of Discovery at Pfizer’s Rare Disease Unit. “We’re not only attempting to address growth, but some of the major complications in early childhood that severely impact quality of life,” says Czech.
Addressing medical issues
Some members of the achondroplasia patient community, however, are wary of treatments for dwarfism, which they don’t see as a disease, but rather a different body type. “Depending on where you go around the globe, achondroplasia families have different attitudes and approaches to the development of therapies,” says Sam Collins, Senior Director Rare Disease, Clinical Research. “However, what is clear is that there are severe complications in childhood, from which no family wants to see their child suffer,” he adds.
But a potential investigative medicine could also address some of the varied cardiovascular, respiratory, metabolic and neurological conditions associated with the condition. People with achondroplasia can have stunted bone growth at the base of the skull and the spine. “There are some serious complications such as sleep apnea, ear infections and compression of the spinal cord that are all related to the skull anatomy,” says Collins. “And it looks like if you address it early enough, you may improve these complications, which cause severe impairment of quality of life,” he adds. “Our focus is on the aspects that really impact the lives of those with achondroplasia, not just trying to increase height.”
In addition, people living with the condition also have day-to-day challenges due to their disproportionately short limbs. Activities like combing their hair or getting dressed can be daily obstacles and therapies that improve these proportions could have a huge impact on the quality of life of the patients.
Reducing receptor activity
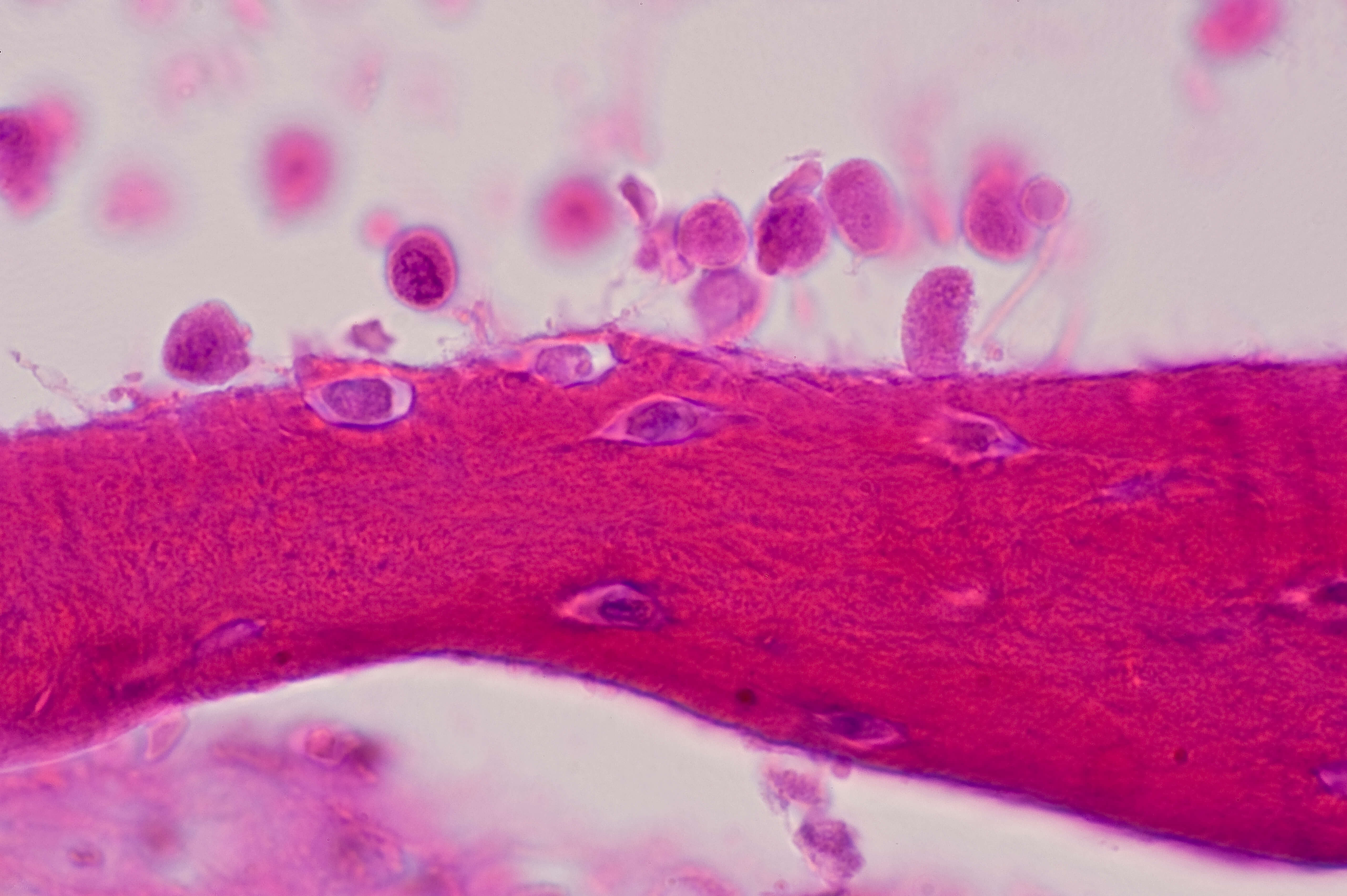
In 2013, a French academic researcher in Nice first discovered this potential therapy for achondroplasia in mouse models. The genetic condition is caused by a mutation on the FGFR3 on chondrocytes, a type of cell that helps our bones elongate. Normally the receptor helps to regulate bone growth, but when it’s overactivated due to this mutation, it hinders normal bone lengthening. The potential therapy is designed to interfere with molecules that activate the FGFR3, and thus increasing the potential for the bones to develop more normal.
Currently, as they ramp up for phase II studies, Pfizer scientists are conducting two "Natural History" studies of children with achondroplasia to get a better understanding of how the condition progresses as the children develop. Unlike more common conditions like diabetes or Alzheimer’s disease, in rare diseases there often is a limited amount of published research on the condition. “You really need to understand your patient population on a clinical and molecular level, so you can deliver a treatment that is meaningful,” says Czech.