Where Do Pandemics Come From?
Fleas seem like just an itchy nuisance for your pets, yet they were responsible for two of the most devastating plagues in human history. The bacteria Yersinia pestis, carried by fleas from rodent to rodent, was responsible for the Plague of Justinian in the sixth century and the Black Death in the 14th century. The Plague of Justinian cost 100 million lives in the Roman Empire, while the impact of the Black Death was as high as 200 million souls across medieval Europe. Now classified as a reemerging infectious disease, plague has taken several thousands lives in the past few years, almost exclusively in developing nations.
Environmental exposures led to previous pandemics
Historically, pandemics were most commonly associated with environmental exposures such as raw sewage, according to Jay Purdy, MD, PhD, vice president and therapeutic area lead in anti-infectives in the department of Global Medical Affairs at Pfizer. Purdy points out that a lack of basic hygiene in centuries past meant people frequently bathed in and drank from feces-polluted rivers and streams.
“The classic example is the cholera outbreak in London in 1854 in which a communal pump was implicated,” he says. “Even though it had this reputation of offering very fresh-tasting water compared to some of the other water sources in London, it was disseminating cholera and killing large numbers of folks there.” Local authorities concluded that an easy solution was the removal of the pump’s handle.
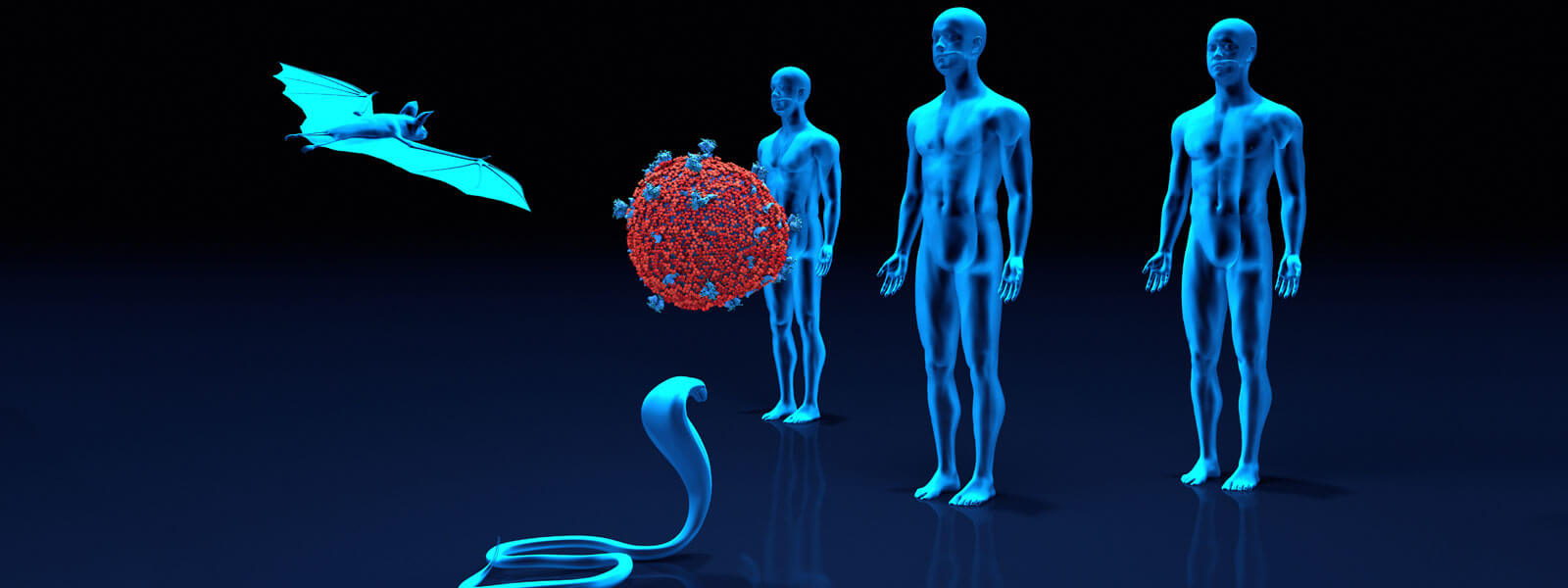
The zoonotic origins of pandemics
More recently, pandemics have tended to occur in a very different way: as a result of spread from animals. Animals as the root cause of pandemics is nothing new--the infamous Black Death, which struck Europe in the 14th century and then again in the 17th century, caused huge death tolls worldwide thanks to fleas that hitched rides on shipboard rats--but now that water supplies have been sanitized and basic hygiene measures understood, modern pandemics jump from animals into human populations.
This century alone, the SARS (severe acute respiratory syndrome) outbreak of 2002-2003, MERS (Middle East respiratory syndrome), which first appeared in 2012, and SARS-CoV-2 (COVID-19) have been identified as likely zoonotic in origin, with host animals such as bats, palm civets, and camels enabling the spread to humans.1 It is bats, however, that Purdy maintains play a central role in modern pandemics; genetic markers demonstrate close associations between bats and the viruses that cause so much human misery.
“Bats are an interesting species in that if you read books on zoonotic spreads and zoonotic risks, they’re probably the number one category, and there’s a number of reasons for that,” Purdy says. “They have the ability to move across large distances and they live in colonies so they spread pathogens readily from one to another, but there’s certainly more than that. There’s something about their genetic makeup that allows them to harbor viruses that can be spread to humans.”
Wild primates also can be vectors for disease. According to Purdy, HIV likely made its way from monkeys and chimpanzees into humans when indigenous people hunted, dressed, and ate primates infected with one of the many simian immunodeficiency viruses in existence.
The origins of COVID-19 have not been definitively determined, leading to a theory among some that the virus was leaked from a laboratory. “While it's possible for pathogens to escape from labs dedicated to their understanding and control, it is unlikely given the safeguards in place," Purdy says. "For SARS-CoV-2, it is much more likely that the virus entered the human population from wild bats.”
Can avoiding certain animals prevent future pandemics?
Despite this risk, bats have an important role to play in our ecosystem. “Bats serve a really important purpose,” Purdy says. “They consume huge amounts of insects, including some that carry things like malaria, yellow fever, and dengue fever. You don’t want to eradicate bats.”
While steering clear of bats and their habitats is generally a good idea in the interest of avoiding disease, Purdy acknowledged that certain cultures have a history of interacting with bats and other potential animal vectors that will make it difficult to prevent future zoonotic outbreaks.
“Are we ever going to be able to avoid all outbreaks?” Purdy asks and answers. “No, I just don’t think that’s the case. There’s always something. The community of bacteria and viruses and protozoa are very good at adapting and becoming better at infecting their hosts.” Combine that with our modern society, he added, with air travel and an increasingly mobile populace, and the potential exists for more rapid disease spread than ever before.
The positive news is that we have potent weapons at our disposal to contain outbreaks once they arise. Vaccine development has advanced by leaps and bounds, with messenger RNA vaccines acting as a tool that can potentially be adapted quickly to combat new pathogens. Nations and their leaders also need to have the will to implement and follow disease-dampening measures that can slow or halt transmission of future outbreaks, Purdy emphasizes: “It’s social distancing, it’s masks, it’s hand washing--things that we used to think didn't make a difference. They do make a difference, to be sure, until we’re able to develop a vaccine and disseminate that vaccine.”
References:
- National Institute of Allergy and Infectious Diseases. “COVID-19, MERS & SARS.” Available at: https://www.niaid.nih.gov/diseases-conditions/covid-19. Last reviewed August 18, 2020.
![]()
![]()
