Got the Flu? It May Be Because of Your Genes
Genetic factors may explain why some people get sick and others avoid infectious diseases.
When flu season strikes, why do some people get sick, some get by without even a slight cough, and an unfortunate few land in the hospital with a severe illness?
We’ve long known that a complicated mix of factors — from age and stress to environment and illness history — can impact whether we get sick and how long it takes to recover. Now a growing area of research, aided by advances in human genome sequencing technology, shows that genetics plays an important role in the immune system’s ability to fight off foreign invaders.
“The benefit of this research is not limited to infectious diseases. It helps us pinpoint functions of individual proteins in our immune system, potentially guiding us to more targeted and personalized medicine for various immunological disorders,” says scientist Wei Li, who is based in Pfizer’s Inflammation and Immunology research unit in Kendall Square, Cambridge, Massachusetts.
Holes in Genetic Armor
One of the leading researchers in this field, Jean-Laurent Casanova of Rockefeller University in New York, focuses on how gene mutations can make certain everyday infections more life-threatening for some children.
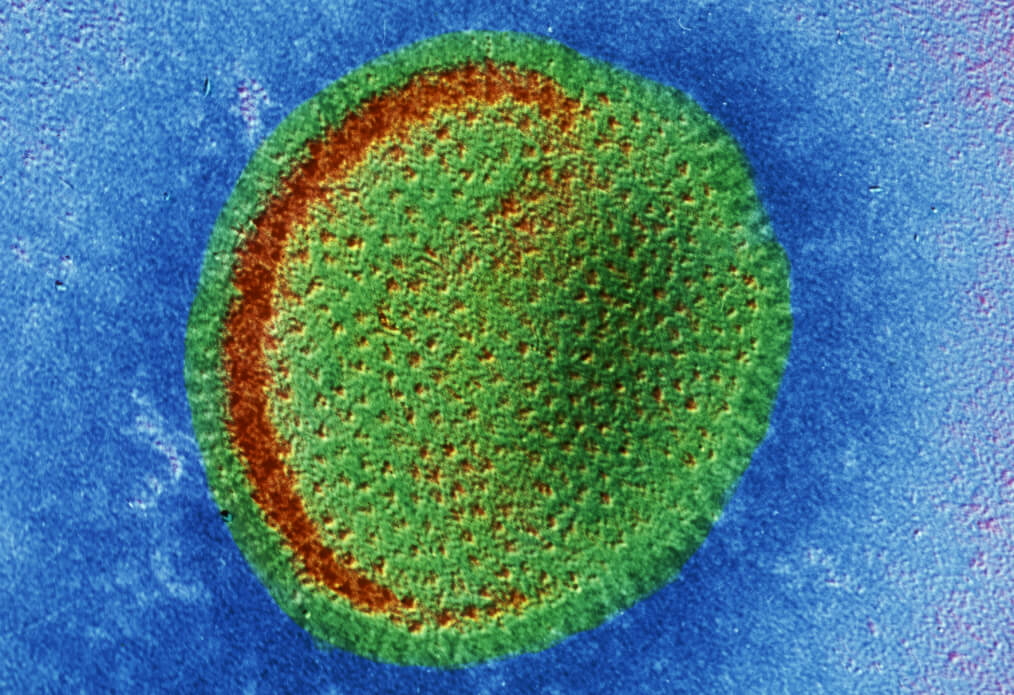
In 2011, one of his patients, a two-year-old French girl, was hospitalized with a severe case of the common flu. Stuggling to breathe, the previously healthy toddler had such acute symptoms that Casanova had a hunch that genetics may be in play. “Infectious diseases of childhood, once thought to be archetypical environmental diseases, actually may be among the most genetically predetermined conditions of mankind,” writes Casanova in a 2015 paper in the Proceedings of the National Academy of Sciences. By sequencing her genome, he found that the girl had mutations on the gene coding for a protein that activates the body’s response to flu viruses, called interferon. In the cells lining her lungs, where the flu virus attacks, she lacked interferon, rendering her unable to fight off the infection.
This genetic defect is rare, according to Casanova, affecting about one in 10,000 people.But over two decades of research, Casanova’s team has also identified other genetic mutations that may make some children more vulnerable to tuberculosis and certain types of fungal and herpes infections.
It’s not just childhood where genetics can have a role in infectious diseases, either. A separate team of researchers studying adults has found that a certain gene mutation makes them more likely to be hospitalized when sick with the flu.
Beneficial Mutations
It’s not all bad news on the genetics of infectious disease front though. Some people may hit the genetic lottery by inheriting genes that make them resistant to a specific infection.
About 20 percent of the population, for example, inherit a mutation on the FU2 gene (which is related to the ABO blood types) that helps them evade the most common strain of the norovirus, also known as the “stomach flu.”
Specifically, mutations on the FU2 gene inhibit the ability to produce special proteins that appear on the surface of cells. The invading norovirus needs these proteins to be able to latch on to and attack our digestive tract cells. Without the cellular entre, they can’t make us sick. Next time you evade a bout of the stomach flu, you may have your gene mutation to thank.
