What Is Hemophilia?
Typically inherited from one or both parents, hemophilia is a rare blood disorder that stops blood from clotting properly. Because people with hemophilia don’t have enough blood-clotting proteins or clotting factors, they may take longer to stop bleeding after surgery or an injury.1
For people living with hemophilia, bleeding can occur spontaneously or from an injury. Internal bleeding is a significant concern, as it can lead to organ damage or death.1,2
Prevalence of Hemophilia
Worldwide, more than 200,000 people live with some form of hemophilia.3 New data, however, indicate that hemophilia might be underdiagnosed. The actual global population with hemophilia could be more than 1.1 million.4 The extent of hemophilia in the United States is unknown, but data suggests that about 33,000 people assigned male at birth are living with hemophilia nationwide.5
The condition most commonly affects those who were assigned male at birth.1 In one study, those assigned female at birth accounted for roughly 18% of mild hemophilia cases and less than 1% of severe cases.6 Hemophilia typically affects white and Hispanic patients, while it is less prevalent among Black and Asian patients.7
Causes and Risk Factors
What Causes Hemophilia?
Hemophilia is often inherited, meaning genetics play a strong role in who develops hemophilia. But in some cases, hemophilia is acquired.2
In most cases, a mutation in the genes responsible for making clotting factors causes hemophilia.2 The genes for factors VIII and IX are only found on the X chromosome, while the factor XI gene is found on chromosome 4.12, 13
Some patients develop acquired hemophilia. This occurs when a patient's immune system attacks clotting factors VIII14 Acquired hemophilia can be associated with:14
- Pregnancy
- Autoimmune conditions such as lupus
- Cancer
- Multiple sclerosis
- Drug interactions
Hemophilia and Genetics
Why is hemophilia more common in those assigned male at birth? The genes for clotting factors sit on the X chromosome, not the Y.1 People with XY chromosomes develop hemophilia if they inherit an altered copy of a gene on their X chromosome. On the other hand, a person with XX chromosomes can inherit an altered copy of a gene on an X chromosome from one parent but receive an unaltered copy on the X chromosome inherited from the other parent. This combination can offer some defense against developing hemophilia.12
People with XX chromosomes who inherit only one altered copy of a gene are known as “carriers.” They sometimes experience hemophilia symptoms and can pass the gene mutations onto their children.1 To develop severe hemophilia C, a person must have parents who both carry the genetic mutation.10 A person can inherit the condition from just one parent, but it’s usually less severe when a patient inherits only one mutated gene.10
Hemophilia Risk Factors
The genetic link to hemophilia focuses on two significant risk factors. People are more likely to inherit the genetic mutations that cause hemophilia when they have:2,5
- A family history of hemophilia
- Only one X chromosome
Hemophilia Prevention
Because the condition is genetic, there’s no way to prevent hemophilia.2 However, patients can take steps to limit the frequency and severity of their bleeding.1,2
- Using caution with certain medications
Aspirin and NSAIDs (ibuprofen and similar drugs) can worsen bleeding in patients with hemophilia.15,16 Medications designed to prevent blood from clotting can also be problematic for those with hemophilia.16 Consulting a healthcare provider can help with informed decisions.
- Keeping teeth clean
Brushing regularly can help prevent gum and tooth disease, which can cause excessive bleeding.17
- Getting regular exercise
Frequent physical activity strengthens muscles and protects joints. Activities such as swimming, walking, or biking can help, whereas contact sports are not recommended.18,19
- Using protective gear
Before engaging in physical activity, it can be helpful to talk to a doctor or physical therapist about what protective gear is appropriate.19
- Getting vaccinated
Following vaccination schedules is recommended.20
The three most common kinds of hemophilia are:
This type is typically inherited, ranging from mild to severe. A mutation of the F8 gene on the X chromosome causes low production of clotting factor VIII, leading to bleeding in the muscles and joints. Patients with XY chromosomes are more susceptible.8 In the United States, new research shows hemophilia type A affects 1 in every 5,000 births of people assigned male at birth—approximately 400 babies annually.5
Known as Christmas disease or factor IX (FIX) deficiency, this inherited form of hemophilia stems from an F9 gene mutation on the X chromosome.9 This results in a lack of clotting factor IX and, as with hemophilia A, it can cause bleeding in the muscles and joints.1,9 Still, it's four times less common than hemophilia A.1
This type of hemophilia is also called Rosenthal syndrome or factor XI deficiency. Factor XI is responsible for helping to set off a critical chain of events: It’s integral to creating thrombin, the protein that converts fibrinogen to a substance called fibrin. In turn, fibrin holds platelets together to form a blood clot.10 Inconsistent with hemophilia A and B, the mutation that causes hemophilia C is located on chromosome 411 It’s mainly autosomal recessive, meaning both parents must carry the gene for a child to inherit the condition. The deficiency affects people born with XX and XY chromosomes equally. Hemophilia C affects 1 in every 100,000 people. In Israel, hemophilia C affects as many as 8% of Ashkenazi Jews.10
Hemophilia Symptoms
Patients may experience hemophilia signs and symptoms, including:1
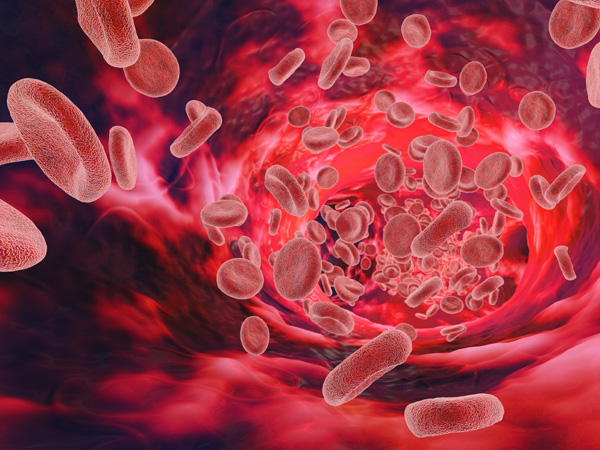
- Bruising and bleeding into the muscles and soft tissues, potentially creating a blood buildup called a hematoma
- Bleeding in the joints, typically the ankles, knees, and elbows. This can cause pain, swelling, and tightness
- Post-shot bleeding (e.g., after intravenous injections or vaccinations)
- Bleeding in the mouth (e.g., at the gum line or after tooth loss)
- Post-circumcision bleeding
- Blood in urine or stool
- Nosebleeds that happen frequently and are difficult to stop
- Head bleeding in infants after a difficult delivery
- Unexplained irritability in infants.21

Hemophilia Complications
Depending on the severity of the case, several complications of hemophilia may arise. Patients should look out for:
- The development of inhibitors: Inhibitors are a type of antibody that can target factor VIII and factor IX, neutralizing their effects.19
- Joint problems: People with hemophilia sometimes suffer joint damage from repeated bleeds.19
- Pseudotumors: A pseudotumor is a hematoma (a pool of blood) that typically develops in muscles adjacent to bones, mostly in the long bones or pelvis. Pseudotumors can pose serious risks if not monitored by a healthcare professional.19,22
- Fractures: Bones can break as joints become damaged from repeated bleeds.19
- Compartment syndrome: A rare but severe complication can arise when bleeding puts pressure on the arteries and nerves within a muscle, potentially causing serious limb injury.23
The severity of the condition has a large influence over potential life span. Hemophilia patients’ life expectancy is six years shorter on average—however, with the advancements of the past 45 years, those estimates are approaching that of the general population.24
Diagnosis and Treatment
Hemophilia Treatment
After receiving a hemophilia diagnosis, patients should consider visiting a comprehensive hemophilia treatment center. These facilities are staffed with doctors and nurses specially trained to provide personalized treatment and education on staying healthy and minimizing health risks.1
With adequate treatment, most patients can expect to live a relatively normal life with little impact on daily activities. However, hemophilia management is often more complex for people who develop an inhibitor, an antibody that makes it difficult to control bleeding.25
Several hemophilia treatments are either under investigation or already available.
- Factor Replacement Therapies
These therapies replace patients’ missing clotting factors with clotting factor concentrates. Clotting factor concentrates can be administered by injection or infusion.26
There are different types of factor replacement products, including:
- Standard half-life (SHL): The half-lives of these replacement products are about 8 to 12 hours for factor VIII and 18 to 40 hours for factor IX.27
- Extended half-life (EHL): These factor VIII replacement products have half-lives about 1.5 times longer than SHL options. EHL factor IX replacement products' half-lives are up to five times longer than SHL alternatives.27
Some people develop inhibitors that prevent their bodies from accepting factor treatment products. These patients require special treatment, sometimes in the form of bypassing agents that circumvent the inhibitor-blocked factors and support clot development.25 - Non-Factor Replacement Therapies
Several medications and therapies are available for hemophilia treatment, including:26
- ACE 910/emicizumab. For patients with hemophilia A, this subcutaneous injection does not include clotting factors, but it may reduce or prevent bleeding incidents.
- Desmopressin acetate. This intravenous injection or nasal spray causes the body's tissues to release factor VIII, using medications similar to naturally occurring hormones. It increases the amount of factor VIII in patients with mild to moderate hemophilia.
- Epsilon Amino Caproic Acid. Delivered as an oral medication or intravenous injection, this hemophilia medication stops clots from dissolving and makes existing clots firmer. It’s typically administered for mouth bleeding.
Hemophilia Prognosis
Life expectancy for people with hemophilia has increased. For example, one study of patients in the Netherlands found that, between 2001 and 2018, people with hemophilia had a median life expectancy of 77 years, which was 6 years lower than the general population of people who were assigned male at birth. This marked an 11-year improvement over the previous hemophilia life-expectancy data, which spanned from 1973 to 1986.24 Patients who receive care in hemophilia treatment centers are 40% less likely to experience death or hospitalization due to their disease.5
Global Impact of Hemophilia

Hemophilia affects patients worldwide. A global report from the World Federation of Hemophilia found that 67% of cases occur in low- and lower-middle-income countries. The study also found that hemophilia can negatively impact employment, with 12% of patients reporting that hemophilia led them to part-time work, extended leave, or unemployment.28 Most people with hemophilia report mobility problems, pain, and bleeding incidents.29
Healthcare costs for people with hemophilia can also be significant. In the United States, the average price tag for managing hemophilia B is greater than $200,000 per patient annually, with the cost exceeding $630,000 for patients with severe hemophilia B.30 In Europe, the average annual per-patient cost of severe hemophilia A and B is about €200,000, according to a study that examined costs in France, Germany, Italy, Spain, and the United Kingdom. Drugs accounted for almost 98% of direct costs.31 In Australia, the average annual per-patient cost for moderate to severe hemophilia A is about €74,000.32
Frequently Asked Questions About Hemophilia
Patients and caregivers will understandably have some common questions about the disorder and how to manage it.
- Is hemophilia dominant or recessive?
Hemophilia is a chromosomally linked recessive disorder, the result of a mutated gene on the X chromosome. Because those assigned male at birth only have one X chromosome, they can develop hemophilia if they inherit the altered gene.2 Carriers, who have only one altered gene, may experience symptoms and pass the mutation down.1
- Can women have hemophilia?
Although comparatively rare,1 people assigned female at birth can inherit hemophilia. A person can inherit X chromosomes with altered copies of genes from both parents. Or a person can inherit an X chromosome with a gene mutation and an X chromosome that does provide protection.12
- Why is hemophilia more common in patients with XY chromosomes?
The genes for clotting factors sit on the X chromosome, not the Y.1 For people with XY chromosomes, inheriting one altered copy of a gene is usually enough to cause the disease. On the other hand, a person with XX chromosomes who inherits an altered copy of a gene on one X chromosome might receive an unaltered copy on the other X chromosome, offering some defense against hemophilia.12
- How common is hemophilia?
Globally, more than 200,000 people live with some form of hemophilia.3 In the United States, the estimated incidence of hemophilia A is 1 in every 5,617 births of people assigned male at birth, who have XY chromosomes. The estimated incidence of hemophilia B is 1 in every 19,283 births of people with XY chromosomes.7 In one study, patients who were assigned female at birth account for roughly 18% of mild hemophilia cases and less than 1% of severe cases.6
- Can hemophilia be prevented?
No, hemophilia cannot be prevented, but patients can take action to limit the severity and frequency of bleeding.1,2
- Is there a cure for hemophilia?
Treatment options can help reduce the frequency and severity of bleeding.26
- How is hemophilia diagnosed?
Your doctor will run diagnostic tests, including blood tests to check for clotting factors. Your care team may also conduct genetic testing.5,33
Find a Pfizer clinical trial for hemophilia at PfizerClinicalTrials.com.
Explore hemophilia clinical trials at ClinicalTrials.gov.
Area of Focus: Rare Disease
Hemophilia is a focus of Pfizer’s Rare Disease Therapeutic Area. Visit the Rare Disease Page.
- References
- What is hemophilia? Centers for Disease Control and Prevention. https://www.cdc.gov/ncbddd/hemophilia/facts.html. Last reviewed July 17, 2020. Accessed August 2, 2022.
- Hemophilia. MedlinePlus. https://medlineplus.gov/genetics/condition/hemophilia/. Last reviewed May 6, 2022.Accessed September 29, 2022.
- Report on the annual global survey 2020. World Federation of Hemophilia. http://www1.wfh.org/publications/files/pdf-2045.pdf. Published October 2021. Accessed August 2, 2022.
- Iorio A, Stonebraker JS, Chambost H, et al. Establishing the Prevalence and Prevalence at Birth of Hemophilia in Males: A Meta-analytic Approach Using National Registries. Ann Intern Med. 2019;171(8):540-546. doi:10.7326/M19-1208
- Data & Statistics on Hemophilia. Centers for Disease Control and Prevention. https://www.cdc.gov/ncbddd/hemophilia/data.html. Last reviewed September 14, 2020. Accessed August 2, 2022.
- Miller CH, Soucie JM, Byams VR, et al. Women and girls with haemophilia receiving care at specialized haemophilia treatment centres in the United States. Haemophilia. 2021;27(6):1037-1044. doi:10.1111/hae.14403.
- A New Study of Hemophilia Occurrence Finds Many More Cases in the United States. Centers for Disease Control and Prevention. https://cdc.gov/ncbddd/hemophilia/features/keyfinding-hemophilia-occurrence-US.html. Last reviewed July 17, 2020. Accessed August 2, 2022.
- Hemophilia A. National Institutes of Health. https://rarediseases.info.nih.gov/diseases/6591/hemophilia-a. Last reviewed November 3, 2018. Accessed August 2, 2022.
- Hemophilia B. National Institutes of Health. https://rarediseases.info.nih.gov/diseases/8732/hemophilia-b. Published November 8, 2021. Accessed August 2, 2022.
- Factor XI. National Hemophilia Foundation. https://www.hemophilia.org/bleeding-disorders-a-z/types/other-factor-deficiencies/factor-xi. Publish date unknown. Accessed August 2, 2022.
- Jayakrishnan T, Shah D, Mewawalla P. Hemophilia C: A Case Report With Updates on Diagnosis and Management of a Rare Bleeding Disorder. J Hematol. 2019;8(3):144-147. doi:10.14740/jh522.
- How hemophilia is inherited. Centers for Disease Control and Prevention. https://www.cdc.gov/ncbddd/hemophilia/inheritance-pattern.html. Last reviewed August 1, 2022. Accessed September 29, 2022.
- Mandal S, Gami S, Shah S. A case report on an extremely rare disease: Factor XI deficiency. Cureus. Published online October 1, 2020. 12(10): e10746. doi:10.7759/cureus.10746
- Haider M, Anwer F. Acquired Hemophilia. StatPearls. National Library of Medicine. https://www.ncbi.nlm.nih.gov/books/NBK560494/. Last reviewed May 1, 2022. Accessed September 29, 2022.
- Arachchillage DRJ, Makris M. Choosing and using non-steroidal anti-inflammatory drugs in haemophilia. Haemophilia. 2016;22(2):179-187.
- Martin K, Key NS. How I treat patients with inherited bleeding disorders who need anticoagulant therapy. Blood. 2016;128(2):178-184.
- Shastry S, Kaul R, Baroudi K, Umar D.. Hemophilia A: Dental considerations and management. J Int Soc Prev Communit Dent. 2014;4(6):147.
- Strike K, Mulder K, Michael R. Exercise for haemophilia. Cochrane Cystic Fibrosis and Genetic Disorders Group, ed. Cochrane Database of Systematic Reviews. 2016;2016(12).
- Mehta P, Reddivari A. Hemophilia. StatPearls. National Library of Medicine. https://www.ncbi.nlm.nih.gov/books/NBK551607/. Last reviewed June 11, 2022. Accessed September 29, 2022.
- Ritchey AK. Administration of vaccines to infants and children with hemophilia. A survey of the region iii comprehensive hemophilia treatment centers. Blood. 2005;106(11):4079-4079.
- Singleton TC, Keane M. Diagnostic and therapeutic challenges of intracranial hemorrhage in neonates with congenital hemophilia: a case report and review. Ochsner J. 2012;12(3):249-253.
- Rodriguez-Merchan EC. Hemophilic pseudotumors: Diagnosis and management. Arch Bone Jt Surg. 2020 Mar; 8(2): 121–130.
- Rodriguez-Merchan EC. Acute compartment syndrome in haemophilia. Blood Coagulation & Fibrinolysis. 2013;24(7):677-682.
- Hassan S, Monahan RC, Mauser-Bunschoten EP, et al. Mortality, life expectancy, and causes of death of persons with hemophilia in the Netherlands 2001-2018. J Thromb Haemost. 2021;19(3):645-653. doi:10.1111/jth.15182.
- Inhibitors and Hemophilia. Centers for Disease Control and Prevention. https://www.cdc.gov/ncbddd/hemophilia/inhibitors.html. Last reviewed July 17, 2020. Accessed August 2, 2022.
- Treatment of Hemophilia. Centers for Disease Control and Prevention. https://www.cdc.gov/ncbddd/hemophilia/treatment.html. Last reviewed July 17, 2020. Accessed August 2, 2022.
- Chhabra A, Spurden D, Fogarty PF, et al. Real-world outcomes associated with standard half-life and extended half-life factor replacement products for treatment of haemophilia A and B. Blood Coagul Fibrinolysis. 2020;31(3):186-192. doi:10.1097/MBC.0000000000000885.
- World bleeding disorder registry 2020 data report. World Federation of Hemophilia. https://www1.wfh.org/publications/files/pdf-1971.pdf. Published 2021. Accessed August 2, 2022.
- Banchev A, Batorova A, Faganel Kotnik B, et al. A Cross-National Survey of People Living with Hemophilia: Impact on Daily Living and Patient Education in Central Europe. Patient Prefer Adherence. 2021;15:871-883. Published 2021 Apr 28. doi:10.2147/PPA.S303822.
- Buckner TW, Bocharova I, Hagan K, et al. Health care resource utilization and cost burden of hemophilia B in the United States. Blood Adv. 2021;5(7):1954-1962. doi:10.1182/bloodadvances.2020003424.
- O’Hara J, Hughes D, Camp C, et al. The cost of severe haemophilia in Europe: The chess study. Orphanet Journal of Rare Diseases. 2017;12(1). doi:10.1186/s13023-017-0660-y.
- Brown LJ, La HA, Li J, Brunner M, Snoke M, Kerr AM. The societal burden of haemophilia A. II - The cost of moderate and severe haemophilia A in Australia. Haemophilia. 2020;26 Suppl 5:11-20. doi:10.1111/hae.14083.
- Diagnosis of hemophilia. Centers for Disease Control and Prevention. https://www.cdc.gov/ncbddd/hemophilia/diagnosis.html. Last reviewed July 17, 2020. Accessed September 30, 2022.
The information contained on this page is provided for your general information only. It is not intended as a substitute for seeking medical advice from a healthcare provider. Pfizer is not in the business of providing medical advice and does not engage in the practice of medicine. Pfizer under no circumstances recommends particular treatments for specific individuals and in all cases recommends consulting a physician or healthcare center before pursuing any course of treatment.
Related Articles
When it comes to making the world a better place for people living with hemophilia—a rare disease characterized by inadequate blood clotting—William Addison doesn’t just talk the talk.1,2 And he doesn’t just walk the walk, either. William hiked the Appalachian Trail—all 2,200 miles of it...
Hemophilia is a rare and life-long bleeding disorder in which the blood does not clot normally. While people with hemophilia can lead fairly normal lives with certain precautions to prevent and control bleeds, managing the condition can be challenging. Those living with hemophilia or caring for...