Scientists Mimic Human Organs on Microscopic ‘Chips’ That Enable Drug Testing
By mimicking the way organs operate in the body, the organ-on-a-chip can offer a more realistic and accurate way to test new drugs.
What if you could better predict an experimental drug’s safety and efficacy— before sending it to clinical trials? A promising new technology that may allow scientists to mimic human organs in a lab is opening the door to that possibility of more accurately and more quickly predicting future efficacy.
This technology, sometimes known as “organ-on-a-chip,” could have an important impact on the complex process of testing drugs before they go into clinical trials.
A More Human Model
The conventional method of testing drugs on human cells — in isolation in a tissue culture plate — has a major shortcoming in that it’s difficult to model the complex interactions those cells have in a living, breathing organism.
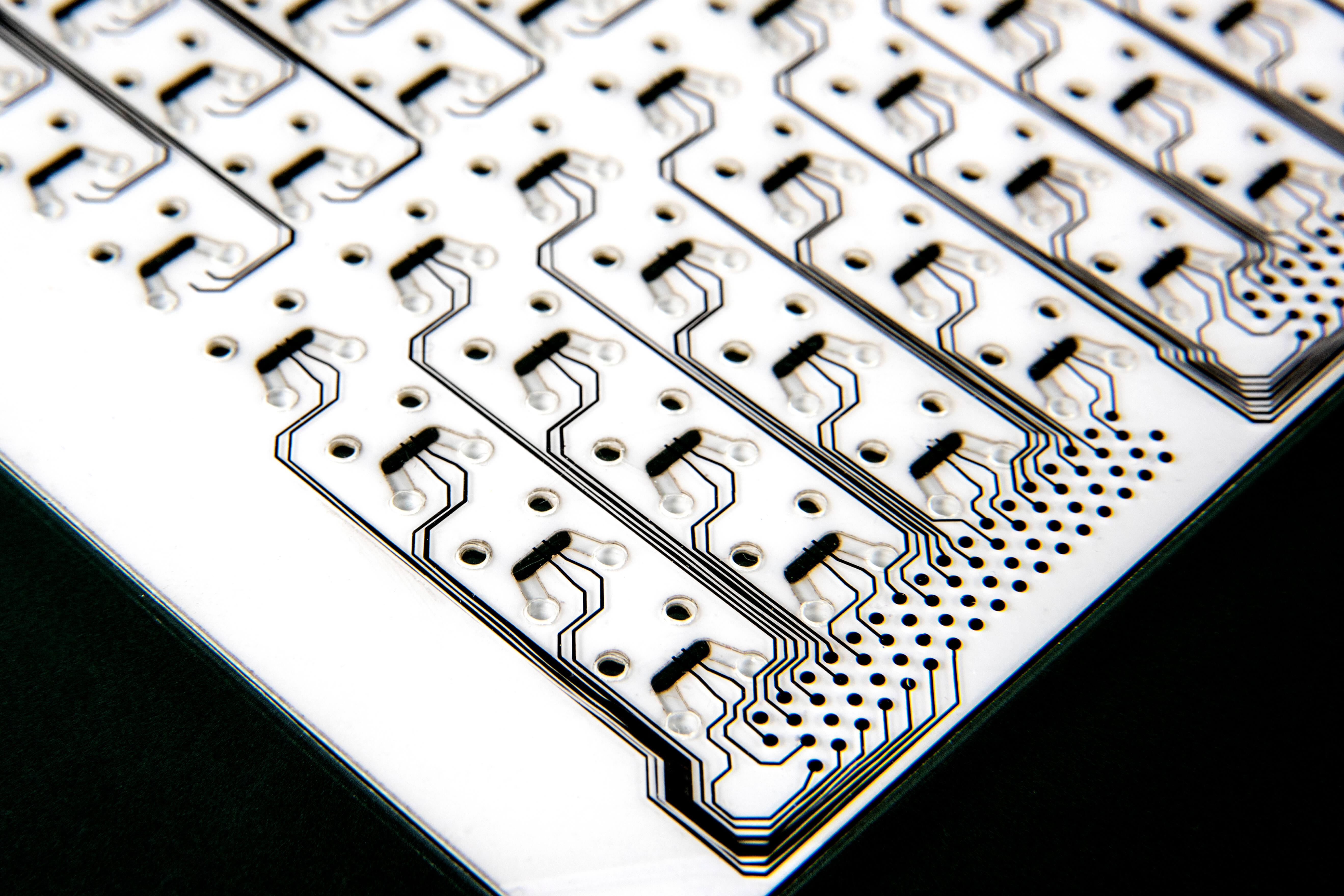
The organ-on-a-chip technology being developed by Draper of Cambridge, Mass., which it calls microphysiological systems (MPS) or human organ systems (HOS), grows human cells on a device made of biocompatible plastic with microscopic structures that simulate the cell’s natural environment in a human body. The structures include channels for controlled fluid flow, and can even model the environment created by blood flow.
Draper recently inked a deal with Pfizer to jointly develop three unique MPS models— for the liver, vascular and gastrointestinal organs.
“We’re trying to build an in vitro model that has the most attributes you can think of as a human organ. A more human model,” said Megan Robinson, director of Scientific Learning for Pfizer’s Worldwide Research and Development at its Groton, Connecticut site.
“If you’re a chemist, you can make the best compound, but if you can’t test it and know how it might work in a real human, it’s for naught,” Robinson added.
Creating Crosstalk
In fact, by linking these organs on a chip together — much as you would build a computer by linking processors — researchers hope to replicate the body’s multi-organ environment. That’s crucial for drug testing because toxicity, and often efficacy, can be a consequence of a series of interactions involving several organs— something known as crosstalk.
“The traditional paradigm is that we have an idea for a target, and we look at it in test tubes or plastic plates, then we move into cells, but we may be only using one cell type,” Robinson said.
In a 2016 study in the journal Lab on a Chip, Draper researchers detailed a portable device using human cells that allowed them to investigate individual organ function and crosstalk between cells for two weeks. The researchers reported success in precisely controlling fluid levels, temperature, and oxygenation to support its use involving drug toxicity and efficacy testing.
Another major advantage of using Draper’s organ-on-a-chip, according to Yvonne Will, head of Science and Technology Strategy in Drug Safety Research and Development at Pfizer Groton and lead scientist for the project, will be that “you can take 96 different drugs and test them at the same time in one chip,” allowing researchers to test potential drug candidates more efficiently.
The Moonshot
If the organs on a chip developed in collaboration between Draper and Pfizer are successful, it could lead to what is considered the “moonshot” of the technology: an entire “human on a chip."
The technology also opens the door to testing drugs tailored to a disease or a specific patient. “Think of it as personalized medicine, as well as personalized toxicology,” Robinson said.
